
Safe Deliveries Study: Increasing Access to Institutional Deliveries Using Demand and Supply Side Incentives
Introduction:
Uganda has a very high maternal mortality rate (438/ 100,000 live births). Only 44% of women attend 4 ANC visits and 57 % deliver in health facilities. Some of the main reasons for not delivering in a health facility include financial limitations, long distances to health facilities coupled with lack of access to transport facilities, and poor quality of care reflected in the frequent shortages of drugs and supplies as well as the poor attitude of health workers who are under facilitated and overworked. Based upon this background, through funding from DFID and the Gates and the Bill and Mellinda Gates foundation, the Future Health Systems consortium and Makerere University School of Public Health in collaboration with the districts of Pallisa and Kamuli implemented an intervention that comprised of both demand (vouchers for transport and maternal services) and supply side initiatives (training health workers and provision of essential equipment, drugs and supplies) to improve access to maternal health services. This intervention was piloted in Kamuli and Pallisa Districts between Dec 2009 and December 2011.
The Research Questions:
- Does providing financial incentives (voucher for institutional delivery and voucher for transport to access antenatal, delivery and postnatal services) increase institutional delivery (in public, private not for profit or private for profit facilities)?
- Does providing financial incentives (voucher for institutional delivery and voucher for transport for antenatal, delivery and postnatal services) increase attendance of antenatal and postnatal care services?
Key findings:
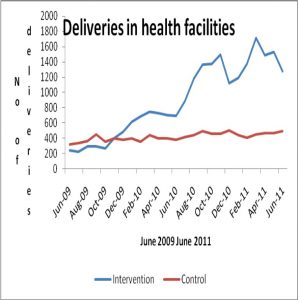
There was an increased up take of antenatal, delivery and postnatal services. It created earnings for transporters, motivated health workers and improved availability of medical supplies. It also increased community awareness about maternal health and gained active support from the community leaders. The incremental costs per additional delivery and PNC attendance were US$23.9 and US$7.6 respectively. The cost per women transported was US$4.6. Cost-effectiveness analysis comparing the status quo and the Schemes most conservative effectiveness estimates revealed favourable cost effectiveness ratios. The Scheme had an incremental cost-effectiveness ratio per DALY averted of US$302 and per death averted of US$20756.
Recommendations:
Based on the findings from this study, the following are recommended:
- Payment of health workers should be increased by introducing a component that is linked to performance, which may provide an incentive for improving the efficiency and quality of services.
- To sustain the initiative, we recommend that districts should work with development partners to promote the economic empowerment of communities through income generating initiatives so that they can contribute to the financing of transport for maternal health services and to buying the requirements needed during delivery.
- Districts should work with the ministry of Health to ensure that health facilities are equipped with the necessary infrastructure, equipment, drugs, supplies and transport for referral cases.
Contact Us:
Email: ekky@musph.ac.ug
