The Expanded Quality Management Using Information Power (EQUIP) Project was created in response to an FP7 EU call to investigate the feasibility and community effectiveness of innovative intervention packages for maternal and newborn health in Africa. EQUIP was designed in the context of persistently high rates of maternal and newborn mortality, despite the availability of evidence-based, affordable and appropriate technical interventions.
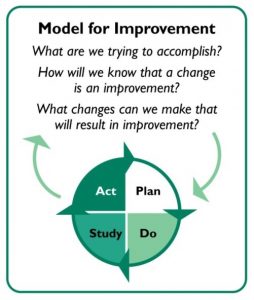
Obstacles to improved survival exist on both the demand (e.g. low utilization) and supply side (e.g. low quality and lack of services). Quality management and quality improvement, defined as structured problem-solving methodology using plan-do-study-act (PDSA) cycles, are increasingly promoted to improve the quality of care. Thus we hypothesized that quality management supported by improved data use, reaching out to communities, and including district managers in the process could improve both utilization and quality of care.
Community QIT during a mentorship session
The overall goal was to assess the feasibility, cost and community effectiveness of an innovative approach of Expanded QM Using Information Power (EQUIP) that links communities and health facilities to increase the quality and utilization of health care services in order to improve maternal and new-born health in rural Uganda and Tanzania.
Project/Study Design & setting
EQUIP utilised a quasi experimental approach with an intervention (Mayuge) and a control district (Namaingo). In parallel to the Quality Improvement (QI) approach, continuous household and health facility surveys were carried out
Results
EQUIP implemented changes in response to a range of improvement topics at district, health facility and community level such as improving facility delivery and Active Management of Third Stage of Labour (AMTSL). The results indicated an increase in live births where mothers received uterotonics within one minute after birth in both countries. In Tanzania, the increase over the project period in the proportion of women with a live birth in the year prior to the survey who received AMTSL was 26 percentage points higher (95%CI;25% to 28%) in the intervention district compared to the comparison district, adjusted for baseline.
In Uganda, the difference was less pronounced at 8% (95%CI; 6% to 9%). In Tanzania our analysis also indicated weak evidence of improvement in early postnatal care (17%: 95%CI; -8% to 17%) and availability of key items for infection prevention (21% difference: 95% CI -4% to 46%). In Uganda we found no evidence of a positive change for the improvement topics early postnatal care and early vaccination of newborns.
Publications
Hanson, C., et al., Expanded Quality Management Using Information Power (EQUIP): protocol for a quasi-experimental study to improve maternal and newborn health in Tanzania and Uganda. Implementation Science, 2014. 9(1): p. 41.
Tancred T, Mandu R, Hanson C, Okuga M, Manzi F, Peterson S, Schellenberg J, Waiswa P, Marchant T, Team TES: How people-centred health systems can reach the grassroots: experiences implementing community-level quality improvement in rural Tanzania and Uganda. Health Policy and Planning 2014.
Marchant T, Schellenberg J, Peterson S, Manzi F, Waiswa P, Hanson C, Temu S, Darious K, Sedekia Y, Akuze J, Rowe AK. The use of continuous surveys to generate and continuously report high quality timely maternal and newborn health data at the district level in Tanzania and Uganda. Implementation Science. 2014 Aug 23;9(1):112
Baker U, Okuga M, Waiswa P, Manzi F, Peterson S, Hanson C, EQUIP Study Group. Bottlenecks in the implementation of essential screening tests in antenatal care: Syphilis, HIV, and anemia testing in rural Tanzania and Uganda. International Journal of Gynecology & Obstetrics. 2015 Jun 30;130:S43-50.
Baker U, Peterson S, Marchant T, Mbaruku G, Temu S, Manzi F, Hanson C. Identifying implementation bottlenecks for maternal and newborn health interventions in rural districts of the United Republic of Tanzania. Bulletin of the World Health Organization. 2015 Jun;93(6):380-9.
Tancred T, Schellenberg J, Marchant T. Using mixed methods to evaluate perceived quality of care in southern Tanzania. International journal for quality in health care. 2016 Jan 27;28(2):233-9.
Tancred T, Manzi F, Schellenberg J, Marchant T. Facilitators and Barriers of Community-Level Quality Improvement for Maternal and Newborn Health in Tanzania. Qualitative health research. 2017 Apr;27(5):738-49.
Tancred T, Marchant T, Hanson C, Schellenberg J, Manzi F. Birth preparedness and place of birth in Tandahimba district, Tanzania: what women prepare for birth, where they go to deliver, and why. BMC pregnancy and childbirth. 2016 Jul 16;16(1):165.
Sedekia Y, Nathan R, Church K, Temu S, Hanson C, Schellenberg J, Marchant T. Data for:” Delaying first birth: an analysis of household survey data from rural Southern Tanzania”
Sedekia Y, Nathan R, Church K, Temu S, Hanson C, Schellenberg J, Marchant T. Delaying first birth: an analysis of household survey data from rural Southern Tanzania. BMC public health. 2017 Jan 31;17(1):134.
Principal Investigator: Prof Stefan Peterson
Co-Investigators: Dr Peter Waiswa, Dr Fatuma Manzi
Funder: European Union
Collaborating Institutions
- Makerere University School of Public Health,
- Karolinska Institutet,
- Ifakara Health Institute,
- London School of Hygiene and Tropical Medicine,
- Evaplan
Contact Emails: pwaiswa@musph.ac.ug; mokuga@musph.ac.ug
